Trigger finger is common with a lifetime occurrence rates of 2.6% in healthy individuals. In diabetics the rate jumps to 10% (Akhtar et al.), but ultimately trigger finger is idiopathic in most cases meaning there is no known cause. Chronic mechanical overuse causing repetitive microtrauma is regarded as the main risk factor.
The diagnosis of trigger finger is based on the medical history and clinical examination with the triggering phenomenon often preceded by pain and joint stiffness (Ryzewicz and Wolf). The ring finger, middle finger, and thumb frequently involved (Makkouk et al.)
Imaging is helpful to help establish the severity of the disease, identifying underlying causes of the triggering, and deciding appropriate treatment options (Orlandi et al.). High resolution diagnostic ultrasound allows for a dynamic assessment of the superficial structures in the hand. Ultrasound also allows for a comparison with the adjacent digits and can be used to guide injections (Orlandi et al.) or pulley releases (Rajeswaran et al.).
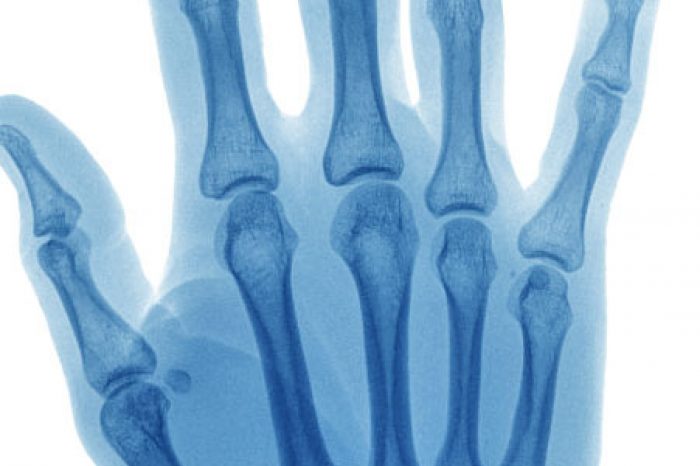
The Anatomy
The annular pulleys (i.e. A1 pulley) are fibrous bands that stabilize the flexor tendons of the thumb and fingers. They are numbered proximal to distal from A1 to A5.
The deep and superficial flexor tendons of each finger insert on the bone of the fingers and thumb, and control finger flexion.
The Pathology of Trigger Finger
Trigger finger is typically due to thickening of the A1 pulley at the level of the metacarpophalangeal joint. Thickening of the A1 pulley narrows the tunnel through which the flexor tendons run, impairing tendon gliding. This local friction can lead to tendon swelling and triggering (Guillin et al.; Vuillemin et al.).
Ultrasound For Diagnosing Trigger Finger
The examination is best performed with high-resolution ultrasound with an experience provider. Dynamic ultrasound imaging during flexion of the thumb and fingers allows for visualization of flexor tendon gliding (Bianchi et al.). The ultrasound can show thickening of the A1 pulley or swelling of the flexor tendons.
References
Akhtar S, Bradley MJ, Quinton DN, Burke FD. Management and referral for trigger finger/thumb. BMJ 2005; 331: 30–33.
Bianchi S, Martinoli C, de Gautard R, Gaignot C. Ultrasound of the digital flexor system: normal and pathological findings. J Ultrasound 2007; 10: 85–92.
Guillin R, Marchand AJ, Roux A, Niederberger E, Duvauferrier R. Imaging of snapping phenomena. Br J Radiol 2012; 85: 1343–1353.
Makkouk AH, Oetgen ME, Swigart CR, Dodds SD. Trigger finger: etiology, evaluation, and treatment. Curr Rev Musculoskelet Med 2008; 1: 92–96.
Orlandi D, Corazza A, Silvestri E, et al. Ultrasound-guided procedures around the wrist and hand: how to do. Eur J Radiol 2014; 83: 1231–1238.
Rajeswaran G, Healy JC, Lee JC. Percutaneous release procedures: trigger finger and carpal tunnel. Semin Musculoskelet Radiol 2016; 20: 432–440.
Ryzewicz M, Wolf JM. Trigger digits: principles, management, and complications. J Hand Surg Am 2006; 31: 135–146.
Vuillemin V, Guerini H, Bard H, Morvan G. Stenosing tenosynovitis. J Ultrasound 2012; 15: 20–28.
Learn about ultrasound-guided A1 pulley release for trigger finger treatment, a minimally invasive procedure with a 97% success rate and fast recovery time. This technique is safer and more effective than traditional
Read MoreTrigger finger, also known as stenosing tenosynovitis, is a common hand condition that affects the tendons in your fingers or thumb. If you're dealing with pain, stiffness, or a locking sensation in your fingers, you
Read More