Trigger finger is a surprisingly common condition that affects millions of people worldwide, yet misconceptions about it persist. Whether you've experienced the frustrating locking and snapping of a finger or are just curious about hand health, it’s essential to separate fact from fiction. In this article, we’ll bust some of the most widespread myths about trigger finger and provide you with the knowledge you need to manage or prevent this condition effectively.
Many assume that trigger finger is solely an age-related condition, but this isn’t true. While the risk increases with age due to factors like repetitive hand movements and underlying health conditions (such as arthritis or diabetes), younger individuals can also develop trigger finger. Infants may even be born with congenital trigger thumb, requiring medical attention early on [Wong et al, 2022; Jia et al, 2023].
If you frequently engage in activities that strain your hands, such as gaming, rock climbing, or playing musical instruments, you may be at risk regardless of your age [Tholl et al, 2022; Guggenheim et al, 2024; Betzl et al, 2020].
It’s true that frequent gripping and hand-intensive activities—such as typing, knitting, or working with tools—can increase the likelihood of developing trigger finger. However, many people who develop the condition do not have jobs or hobbies that overwork their hands [Gorsche et al, 1998; Moore, 2000; Shen et al, 2019].
Underlying health conditions like diabetes, rheumatoid arthritis, and thyroid disease can predispose individuals to trigger finger by causing inflammation and thickening of the tendon sheath. Genetic factors may also contribute, meaning some people may develop trigger finger even without excessive hand use [Guggenheim et al, 2024; Currie et al, 2022; Shen et al, 2019].
Some people experience occasional stiffness or clicking in their fingers that resolves with rest or lifestyle changes. However, for many, trigger finger worsens over time, leading to more frequent locking, pain, and loss of mobility.
Ignoring persistent symptoms can lead to complications, including permanent stiffness and reduced finger function. While corticosteroid injections and splinting are effective first-line treatments for trigger finger, patients with recurrent or severe symptoms may benefit from early surgical release [Yanko et al, 2025; Currie et al, 2022; Hutchinson et al, 2021].
Surgery is an effective option for severe cases of trigger finger, but it is far from the only treatment [Yanko et al, 2025; Ferrara et al, 2020; Atthakomol et al, 2023; Huisstede et al, 2018]. Many people experience relief through conservative approaches, including:
If conservative methods don’t work, minimally invasive procedures such as percutaneous release may be an option before considering traditional surgery.
While pain is a common symptom, not everyone with trigger finger experiences discomfort. Some may notice clicking or snapping when bending their finger but feel little to no pain. Others might have swelling or difficulty straightening their finger without any significant discomfort [Yanko et al, 2025].
Even if your trigger finger isn’t painful, it’s still important to monitor symptoms and seek medical advice if they worsen or interfere with daily activities.
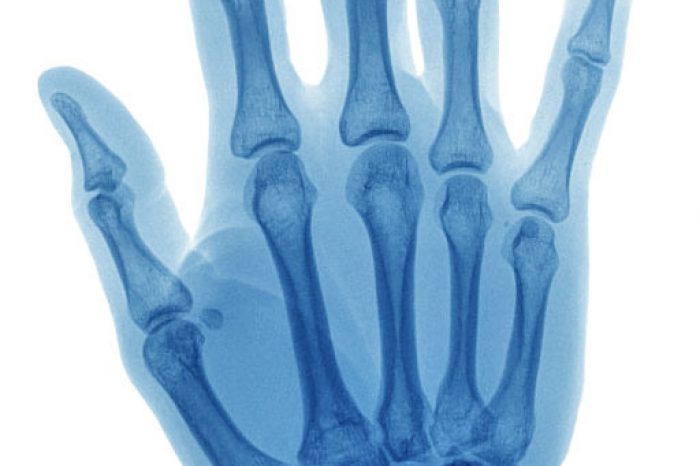
People often assume that trigger finger is just another form of arthritis, but that’s not the case. Arthritis is a broad term that refers to joint inflammation and degeneration, whereas trigger finger is caused by a thickening or inflammation of the tendon sheath, restricting smooth movement.
There is a clear association between osteoarthritis and trigger finger, but this does not establish a direct causative relationship [Guggenheim et al, 2024; Su & Gau, 2024; An et al, 2024]. That said, individuals with arthritis—especially rheumatoid arthritis—are at a higher risk of developing trigger finger due to chronic inflammation affecting tendons and joints.
Some preventive measures can reduce your chances of developing trigger finger, but they don’t provide complete immunity [Huisstede et al, 2018; Yanko et al, 2025]. These include:
Despite these precautions, genetic predisposition and other factors beyond your control may still contribute to developing trigger finger. Trigger finger affects approximately 2% of the general population and up to 20% of adults with diabetes, indicating that underlying health conditions significantly contribute to its development [Currie et al, 2022]. This suggests that even with risk reduction strategies, individuals with predisposing conditions remain susceptible.
If you notice persistent stiffness, clicking, or locking in your fingers, don’t ignore it. Seeking early intervention can prevent complications and help you maintain optimal hand function. A healthcare professional can assess your symptoms and recommend the best course of action, whether that’s physical therapy, medication, or a more advanced treatment.
Trigger finger may be frustrating, but understanding the facts empowers you to take action. By debunking these common myths, you now have the knowledge to identify symptoms, explore treatment options, and take proactive steps to protect your hand function.
Learn more:
(781) 591-7855
20 Walnut St
Suite 14
Wellesley MA 02481
Learn about ultrasound-guided A1 pulley release for trigger finger treatment, a minimally invasive procedure with a 97% success rate and fast recovery time. This technique is safer and more effective than traditional
Read MoreTrigger finger, also known as stenosing tenosynovitis, is a common hand condition that affects the tendons in your fingers or thumb. If you're dealing with pain, stiffness, or a locking sensation in your fingers, you
Read More